Hospital: Hospital Universitario de Basurto.
Nº: C2019-137
Aut@r o Autores: P. Diez Fores, M. Legorburu Toña, G. Elizundia Lopez, J. Gomez Muga, M. Grau Garcia, M. Perez Bea.
Presentación
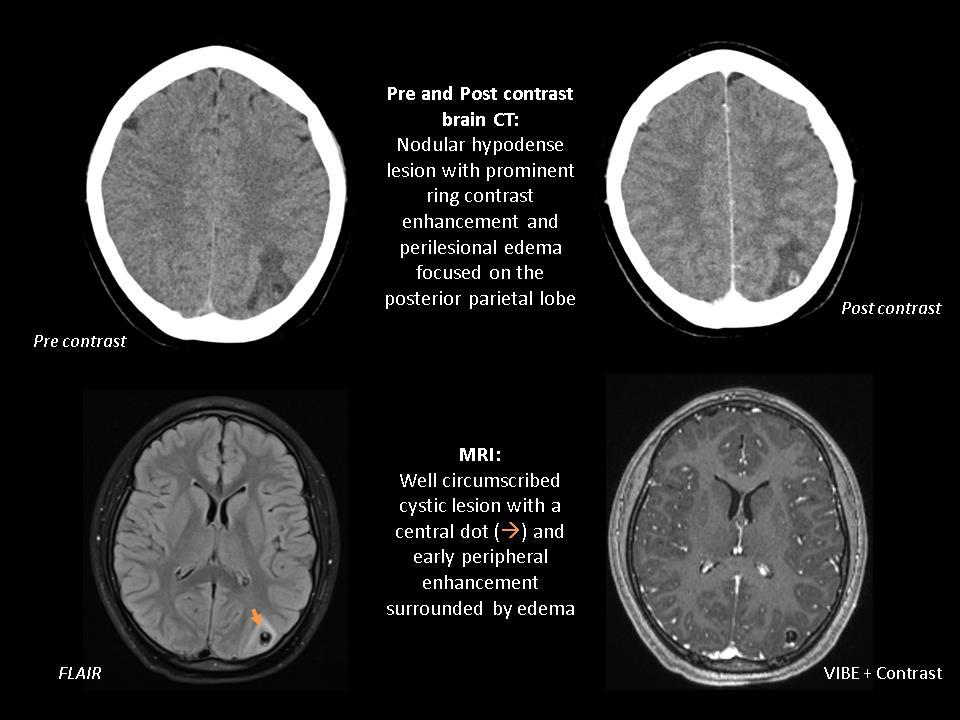
A 16 year-old woman natural from Ecuador, resident in Spain for 9 years, presented to the emergency department with occasional vomiting and two sudden attacks of seizures. The seizures were generalized and tonic-clonic, lasted for about 2 minutes each time and they were not associated with other symtomatology. The patient had neither relevant medical history nor family history of epilepsy and denied toxic abuse. Physical examination revealed an hypersomnolence afebrile woman, with no other relevant clinical features. Single selected pre and post contrast Computerized Tomography (CT) images of the brain, showed a nodular hypodense lesion with prominent ring contrast enhancement and surrounded by vasogenic edema focused on the posterior parietal lobe. Follow-up Magnetic Resonance Imaging (MRI) demonstrated a well circumscribed cystic lesion with a central dot and early peripheral enhancement surrounded by edema.
Discusión
The previously presented case illustrates a neurocysticercosis disease. Neurocysticercosis is a neurologic parasitic disease caused by the encysted larva of the tapeworm Taenia solium, acquired through fecal-oral contamination, and is the parasitic infection that most frecuently affects the central nervous system in humans. It is the most common cause of acquired epilepsy in endemic areas, and nowadays as a result of globalization neurocysticercosis is becoming increasingly prevalent in industrialized countries as well. Imaging findings in neurocysticercosis depend on the location (subarachnoid, parenchymatous or intraventricular) and vary with the stage of cyst development. The early vesicular stage is typified by a smooth thin-walled cyst that is CSF-like on CT and MR images, absence of enhancement and often a mural nodule, which represents the viable larval scolex and gives the characteristic sign of the "cyst with a dot". When cyst degeneration begins, colloidal-vesicular stage, and host inflammatory response ensues, pericystic edema and cyst wall enhancement are present. As the degeneration progresses, granular-nodular stage, the cyst decreases in size and transforms into a smaller nodular lesion. Finally, in the residual stage, small calcified granulomatous lesions are seen. the differential diagnosis for neurocysticercosis includes abscess, tuberculomas, neoplasm (primary or metastatic), and other parasitic infections. Treatment and prognosis is controversial and depends on the form and type of disease, as well as the location and number of cysts, the symptoms, and associated complications.
Conclusión
Neurocysticercosis has a variable neuroimaging features and the early diagnosis can be challenging, so that, radiologists must be aware of its variable imaging appearance and the multiple differential diagnosis for a timely diagnosis and appropriate management.
Bibliografía
- Kimura-Hayama ET, Higuera JA, Corona RC, Chávez LM, Perochena A, Quiroz-Rojas J et al. Neurocysticercosis: Radiologic-Pathologic correlation. RadioGraphics 2010, 30: 1705-1719 - Lerner A, Shiroishi MS et al. Imaging of Neurocysticercosis. Neuro